It has been almost a year since we won the NHS Pay 15 demand at Junior Doctors Conference last year (watch from 1.54 here). This was in the context of repeated below-inflation pay awards, minimal pay requests from the BMA, a growing NHS Pay 15 campaign across multiple unions, and heavy opposition within the BMA.
This year, our arguments about Pay Restoration have become more widely accepted on the Junior Doctors Committee, and our efforts with Medics4PayRestoration and then Doctors Vote have borne some fruit in terms of doctor-created graphics. We will be proposing a motion for full pay restoration at this year’s conference.
So why has the BMA been so slow to put this demand out on social media? Why have they not written to the government with this demand? What has the Broad Left been doing since it passed?
The BMA centrally is now doing some campaigning work, with a webpage, some graphics, a letter-to-MPs tool. Whilst we remain critical of the inadequacy of this work, it is a significant change. It is worth examining what had to happen to get here.
Sorry – this is a long read!
March 2021 Council Meeting
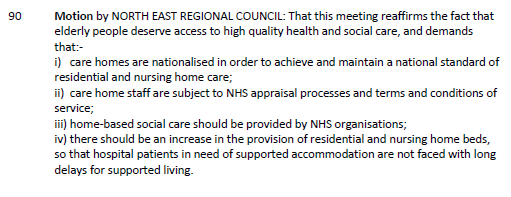
BMA Council has not withdrawn from the DDRB as ARM demanded in 2020, due to concerns about the impact on Devolved Nations and smaller Branches of Practice. Other elements of that motion have not had action taken on them.
The Broad Left and some allies on Council submitted a motion and paper to March 2021 Council
Only parts ii) and iii-i) pass.
Junior Doctors Conference May 2021
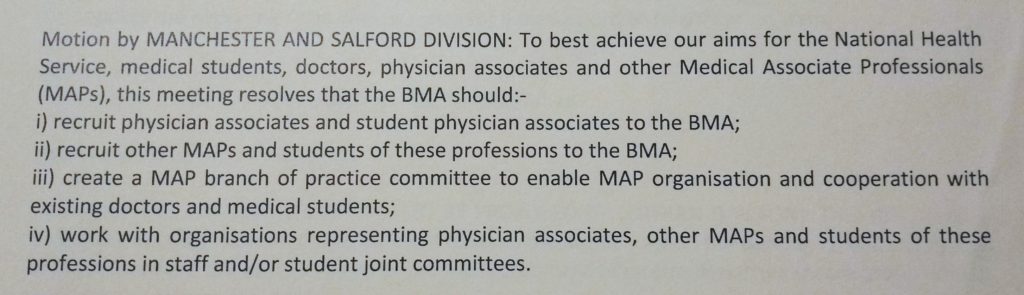
The North West motion from Emma Runswick is composited (merged/compromised into one motion) with a Yorkshire motion to produce this (31 in the agenda here):
You can watch the debate from 1.54 here. It was proposed by David Smith from Yorkshire. Multiple Broad Left members spoke in favour. Part vi) fell due to a requirement to have a two-thirds majority on issues of significant financial cost.
June 2021 JDC Meeting
Broad Left members of JDC gathered the assent of one-third of JDC members to request an additional meeting of JDC to discuss pay strategy, as required in the Standing Orders. Without evidence or warning, we were publicly accused of including members’ names without consent. and a “Lessons Learnt” review was conducted. Despite requests, no evidence and no report from the “Lessons Learnt” review has been offered to members of the Broad Left. Over half of JDC members subsequently voted to have an additional meeting to discuss pay strategy when offered by the Chair of JDC. Two JDC meetings occurred in June, one wholly devoted to pay strategy discussion.
Usually the first meeting of JDC after the Junior Doctors Conference adopts the policies passed at conference. At this meeting, a motion to reject the pay motion was heard. Devolved Nations representatives made clear they would not uphold the policy regardless of whether it was adopted or not. We won the argument and the policy was adopted.
We voted on a series of options and agreed to survey the membership on industrial action if the DDRB and government gave us nothing additional in the 2021 pay round.
October 2021 JDC Meeting
In October, we received the results of that survey. Turnout was ~6,000, and while 96% said the pay offer was unacceptable, that turnout didn’t show that we were yet ready for industrial action of the scale needed to win a 15% pay uplift for doctors in England. JDC outlined a good plan of what was required to build a pay campaign and readiness amongst our members, including education on the key issues, and training for reps and activists. This would draw comparisons to costs of living e.g. fuel and food costs to demonstrate losses against inflation. We agreed to discuss balloting again before the end of the session. We also agreed to withdraw from the DDRB process in England.
December 2021 JDC Meeting
In December, despite the good work JDC and JDC executive had done in outlining what we wanted, the work completed was minimal. We received a short document from the communications team, an outline of a communication and industrial strategy. Key messages included the effect of the pandemic, the lack of award in 2021, and then the pay depreciation we have seen. It planned an activist training session in January, with heavy emphasis on lobbying; member webinars in late Feb/early March, including wider content on financial issues such as coping with higher cost of living and creation of a “strong visual look”; then a campaign for a specific pay ask to the DDRB, which we have withdrawn from.
We were asked whether we should ask the Government not to seek “comments and observations” from the DDRB, and what JDC’s £% ask was for 2022-2023.
We believe the questions were unnecessary and the outline plan misguided: we have withdrawn from DDRB and we knew our ask was 15%. We deserve pay restoration regardless of the pandemic, and many find this focus inappropriate given the widespread trauma. We want to win pay restoration, not just cope with a depreciated income. We know the DDRB will follow the government remit, which is why we have withdrawn from it and are choosing to focus campaigning on the government. Constantly having the same discussions is exhausting.
There were no materials drafted, no KPIs for comms, and no industrial strategy. The discussions at JDC and exec might as well not have occurred for how little there was of them. We did not want a public facing campaign, but assistance to engage our colleagues with a campaign for partial pay restoration. Members of the Broad Left criticised the ongoing “frontline” branding, the lack of materials and the plan for corporate branding. We requested that member-made materials could be checked and circulated by BMA, including infographics and memes which addressed our issues. We wanted shareable versions of our briefing papers which outline the numbers so members could read and make their own contributions on new/social media. We wanted an FAQ which could develop iteratively with activist feedback.
We needed to talk about the plan to win – the industrial action plan: what we are asking for; what the risks are and how we will mitigate them as a union; what taking action could deliver. We highlighted the complete lack of structure testing – i.e. there was no plan to check how ready we were before deciding whether or not to ballot.
We were told this was taken on board and that we would be closely involved with further development. JDC has seen nothing further.
In late January, Emma Runswick was asked if she was free on 15/2/22 for a planned pay activism webinar. She got more information about this the week prior, with suggestions that we discuss successful local organising in the round.
The Webinar: mid-February
We promoted the webinar best we could – including on twitter, facebook, reddit, discord, whatsapp cohort groups. We believe the promotion was insufficient. Approximately 80 attended. Questions were understandably hostile given the lack of progress in the campaign, rising inflation and pay depreciation over the last 15 years. Staff worked to pass questions through that were upvoted, regardless of the hostility, which we believe was correct. We have not seen all the questions or comments, but JDC have since been informed that some were abusive. We have asked to see these.
Emma presented a brief upskilling session on Structured Organising Conversations, but the webinar was one-way in the context of mostly information giving. The website landing page has been created and an activism network set up, with materials for sharing with colleagues and educating promised soon.
The website links to a good briefing and has clear infographics. Do have a look:
Fair pay for junior doctors in England
March 2022 JDC Meeting
In March, JDC was due to have an update on pay campaign activity, see feedback from the webinar event, and discuss what resources were needed. Survey data, requested by other branches of practice, was presented about the public’s view of doctors’ pay campaigning. Communications teams asked JDC some strategy questions about timing, separation from the broader BMA campaigning, straplines and similar.
There were still no materials, no KPIs, no plan for member-led resources, and so on. Industrial strategy is mostly absent from discussion, except to say that industrial action is a tool to get to negotiation. Criticism was heavy.
Now
We are getting progress – graphics with the graph have been released, posters, the webpage and the write-to-MPs tool. Broad Left members of JDC are happy that we are making slow progress and critical of shortcomings of the BMA output. This is now being received well.
However, we continue to do our own work, which does not rely on the slow internal mechanics of the BMA. That work is primarily in our workplaces. We also continue work with Medics4PayRestoration and Doctors Vote, who have wonderful volunteer graphics-creators.
What Now?
Educating Colleagues Ourselves
- Medics4PayRestoration has set up some social media and created infographics for sharing, discussing and building on. @Medics4PayRestoration | Linktree
- Follow Doctors Vote on social media for good graphics to share
Changing policy
- Junior Doctors Conference is coming up this Saturday!
- Please consider lobbying your JDC representatives to vote in favour of “Comp 1” and tell your colleagues about it in work. Having discussions and arguments about this, and convincing colleagues of the need for action on pay is crucial
Elections
- JDC elections will happen at ARM in June and in regions and devolved nations in the summer
Completing our own Structure Test
- Medics4PayRestoration have created a petition which we can use as a test of will building over time Junior Doctors Pay Restoration petition